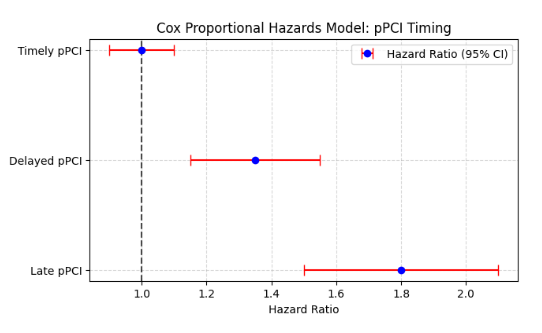
Figure 1: Cox Proportional Hazards Analysis of pPCI Timing and Survival Risk
Primary percutaneous coronary intervention (pPCI) remains the gold standard for treating ST-elevation myocardial infarction (STEMI), yet disparities in treatment timelines, clinical profiles, and outcomes persist between patient groups. A comparative analysis between Group I (n=59) and Group II (n=45) revealed a predominance of male participants in both cohorts, with 84.74% in Group I and 93.33% in Group II. Despite a non-significant difference in sex distribution (p=0.896), significant variations emerged in cardiovascular risk factors. Hypertension (HTN), diabetes mellitus (DM), dyslipidemia (DL), and chronic kidney disease (CKD) were notably higher in Group I, with smoking history and family history of coronary artery disease (CAD) also significantly greater (p=0.003). Clinically, anterior STEMI was more frequent in Group I (50.84% vs. 8.98%), whereas inferior STEMI was more evenly distributed (49.15% vs. 37.28%). Although cardiogenic shock rates were higher in Group I (32.20% vs. 20.33%), this difference was not statistically significant (p=0.60). Killip classification assessments showed comparable distributions across severity classes. Treatment modalities varied considerably, with Group I utilizing low molecular weight heparin (LMWH) at a higher rate (74.57% vs. 0%), while Group II relied more on streptokinase (55.56% vs. 10.16%), though these differences lacked statistical significance. A major discrepancy in the time interval from symptom onset to first medical contact (FMC) was observed, with only 2.22% of Group II patients presenting within three hours compared to 35.59% in Group I, highlighting delayed care-seeking behavior (p=0.002). Total ischemic time comparisons showed a mixed pattern, with no significant disparities. Angiographic findings identified single-vessel disease (SVD) as predominant in both groups, though multi-vessel involvement differed slightly. The left anterior descending (LAD) artery was the primary culprit in 61.01% of Group I and 33.89% of Group II, with no statistical significance.
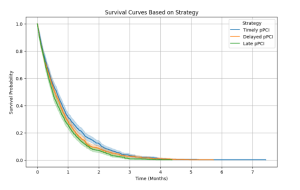
Figure 2: Survival Curves for Different pPCI Strategies Over Time
TIMI flow post-procedure, a critical determinant of reperfusion success, revealed a stark contrast, with 76.27% of Group I achieving TIMI III flow compared to only 48.89% in Group II (p=0.02), underscoring superior post-procedural outcomes in Group I. Post-procedural complications such as bleeding were significantly higher in Group II (28.89% vs. 10.16%, p=0.04), while rates of cardiogenic shock, ventricular fibrillation, and mortality remained comparable. At the three-month follow-up, adverse outcomes like recurrent myocardial infarction, heart failure, and mortality showed marginal differences, reinforcing the importance of early intervention. Further stratification of Group I based on FMC-to-balloon time demonstrated a direct correlation between delayed pPCI and increased complications, with cardiogenic shock and mortality rates escalating from 16.67% to 30.00% and 5.56% to 25.00%, respectively, as treatment delays extended beyond 180 minutes. Hazard ratio (HR) analysis further confirmed that early pPCI conferred the best survival outcomes, with the lowest HR for death (1.3, adjusted HR 1.1) compared to delayed and late pPCI groups. These findings emphasize the urgent need for optimized STEMI management, reducing pre-hospital delays, and ensuring timely pPCI to improve survival and minimize post-procedural complications.